Pregnancy is full of “what-if” questions — and food is one of the biggest. The good news: most risky foods are easy to spot or substitute. Below I explain exactly what to avoid, why it matters, and practical, delicious swaps you can use today. (Clear sources are included so you can check the official guidance.) CDC+1
When I was pregnant with my first baby, I remember standing in the grocery aisle completely overwhelmed — scanning labels, googling “can I eat feta?” and texting my OB every other week. It felt like every food I loved suddenly came with a rule. Over time, I realized pregnancy nutrition isn’t about restriction, it’s about smart swaps and mindful choices. Once I learned what to avoid and what to replace it with, grocery shopping and dining out became much less stressful. I could still enjoy creamy cheese (just pasteurized!), satisfy sushi cravings with veggie rolls, and sip cozy herbal teas instead of coffee. That shift made me feel empowered instead of anxious — and that’s exactly what I want other moms-to-be to experience too. 💛
1) Alcohol — avoid completely (no safe amount)

Why it’s risky: Alcohol crosses the placenta and can harm fetal brain and organ development. Major obstetric organizations say there is no known safe amount of alcohol during pregnancy. ACOG
What to eat/drink instead: Sparkling water with lime, non-alcoholic mocktails (check labels — some contain small alcohol traces), herbal teas (see below).
Practical tip: If you’re offered a drink, order a sparkling water with a lemon wedge — looks the same socially without the risk.
2) High-mercury fish — limit or avoid specific species

Which fish to avoid: shark, swordfish, king mackerel, tilefish, and bigeye tuna are commonly singled out for high mercury. Mercury can harm fetal brain development. The FDA/EPA list shows which species to avoid and which are safer choices. U.S. Food and Drug Administration
Safe swaps: salmon, trout, sardines, haddock, shrimp — aim for 8–12 oz (about 2–3 servings) of low-mercury fish weekly for omega-3 benefits. U.S. Food and Drug Administration
Practical tip: When eating tuna, prefer canned light tuna over albacore (white) tuna; limit albacore to smaller amounts. If in doubt, choose a low-mercury fish or skip that dish.
3) Raw or undercooked seafood — avoid sushi & raw shellfish

Why it’s risky: Raw fish and shellfish can carry bacteria, parasites or viruses that cause foodborne illness (which can be more severe in pregnancy). Ceviche and raw oysters are included here. CDC+1
What to eat instead: Cooked sushi-style (e.g., vegetable rolls, cooked shrimp/tempura rolls) or fully cooked seafood dishes.
Practical tip: Ask the server if the fish is fully cooked; avoid “cold smoked” labeled fish unless it’s part of a cooked dish.
4) Raw or undercooked eggs (and raw-egg foods)

Why it’s risky: Raw eggs can carry Salmonella. Foods like homemade mayo, hollandaise, tiramisu, raw cookie dough and some dressings may contain raw eggs. Mayo Clinic
What to eat instead: Use pasteurized eggs or pasteurized egg products, buy prepared dressings, or enjoy fully cooked egg dishes (yolks firm).
Practical tip: When baking or making desserts at home, use pasteurized eggs if the recipe calls for uncooked/partially cooked eggs.
5) Undercooked / rare meat & poultry

Why it’s risky: Under-cooked meats can transmit bacteria (Salmonella, Campylobacter) and parasites (Toxoplasma) that are riskier during pregnancy. Cook meats to safe internal temperatures (USDA guidance). Mayo Clinic+1
What to eat instead: Well-cooked meats; use a food thermometer (ground meats to 160°F / 71°C; poultry to 165°F / 74°C).
Practical tip: Avoid rare burgers and ask for steak or other meats to be cooked through (or choose fully cooked protein options).
If the idea of giving up a flaky, creamy or crunchy favorite makes you sigh — breathe. Small swaps can keep food vibrant, not boring.
6) Unpasteurized milk, juices and soft cheeses

Why it’s risky: Unpasteurized (raw) dairy can carry Listeria and other bacteria. Soft cheeses that don’t say “made from pasteurized milk” (e.g., some brie, camembert, queso fresco, panela) are commonly implicated in pregnancy listeriosis. nhs.uk+1
What to eat instead: Cheeses labeled “made from pasteurized milk” (cheddar, mozzarella, cream cheese are usually OK when pasteurized), pasteurized milk and juices.
Practical tip: When eating at markets or traveling, ask vendors whether dairy is pasteurized. If the label’s unclear, skip it.
7) Deli meats, hot dogs, refrigerated pâtés — unless heated through

Why it’s risky: Ready-to-eat refrigerated meats (cold cuts, hot dogs, refrigerated pâtés) can harbor Listeria, which is more dangerous in pregnancy (can lead to miscarriage, stillbirth, preterm delivery). The CDC and FDA recommend avoiding these unless steamed/hot to 165°F. CDC+1
What to eat instead: Fresh roasted chicken, tuna (canned; limit per fish guidance), or deli meats reheated until steaming.
Practical tip: If you must eat a deli sandwich, request that the deli heat the meat until it’s steaming — or reheat it yourself at home.
8) Raw sprouts

Why it’s risky: Sprouts grow in warm, humid conditions ideal for bacteria (Salmonella, E. coli, Listeria). Raw sprouts (alfalfa, mung bean, clover) have been repeatedly linked to outbreaks. CDC Archive+1
What to eat instead: Cooked sprouts (cooked thoroughly kills bacteria) or crunchy alternatives like shredded carrot, cucumber, or lightly blanched beansprouts.
Practical tip: Check salads, sandwiches and prepared foods for sprouts — ask for them to be left off.
9) Excessive caffeine & some herbal supplements/teas

Caffeine: Most guidelines recommend limiting caffeine to <200 mg/day during pregnancy (about one 12-oz cup of coffee; guidance varies slightly by agency). Higher intakes have been linked to growth restriction and possibly miscarriage in some studies. ACOG+1
Herbal supplements/teas: Not all “herbal” products are safe. Some herbs (black cohosh, dong quai, pennyroyal, etc.) may stimulate uterine activity or have unknown risks — avoid herbal supplements unless your provider clears them. American Pregnancy Association+1
What to do instead: Choose decaf or low-caffeine drinks, limit green/black tea, and use safe, pregnancy-friendly herbs like ginger or peppermint for nausea only in moderation and after checking with your provider.
Practical tip: Read supplement labels; “natural” ≠ safe. Tell your prenatal provider about any herbal product you take.
10) Liver & very high-vitamin A foods
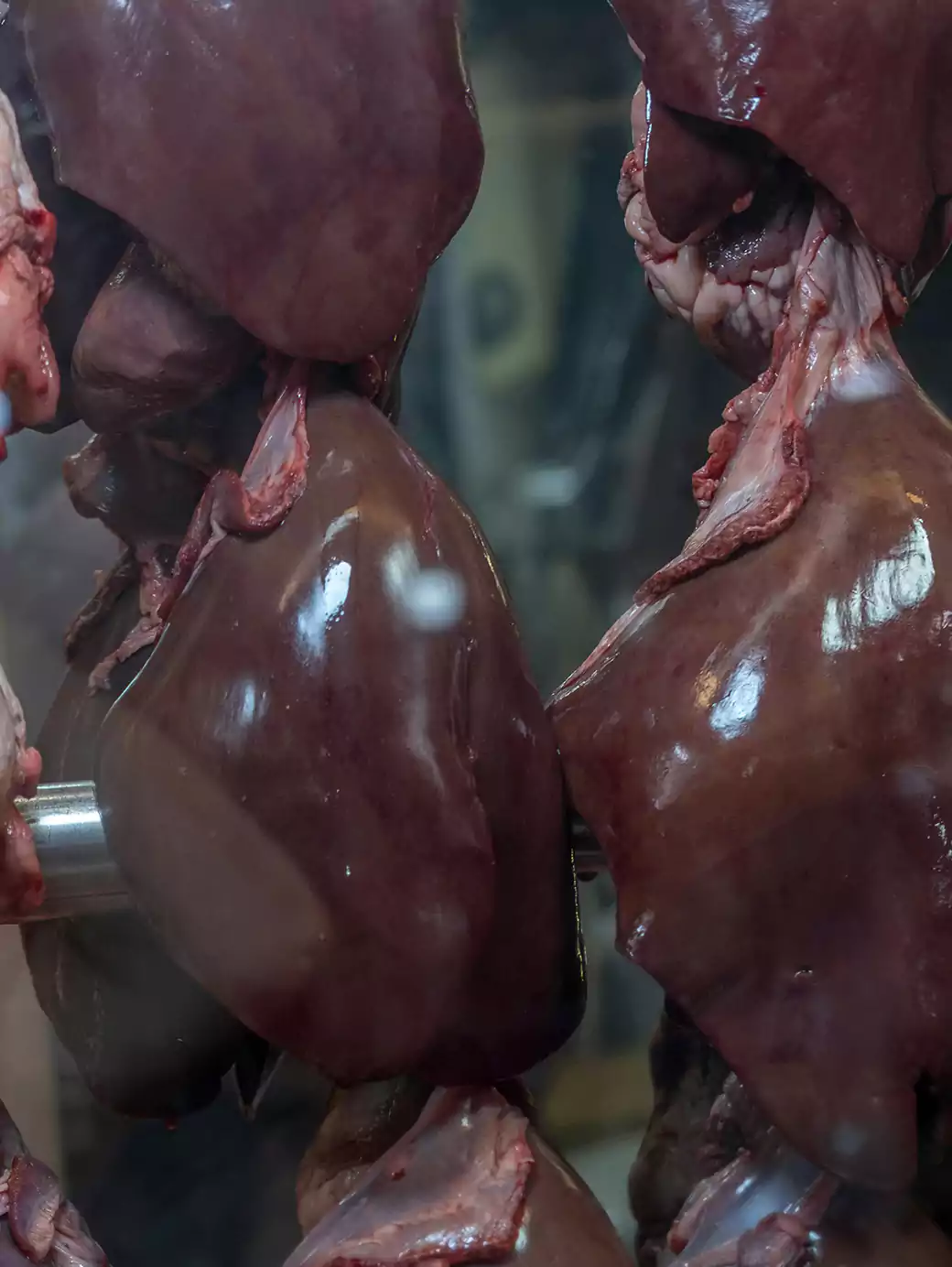
Why it’s risky: Liver and certain liver products (pâté) contain high amounts of preformed vitamin A (retinol). Excessive retinol in early pregnancy is associated with birth defects. Avoid daily or heavy liver intake; check supplements for preformed vitamin A. RCOG+1
What to eat instead: Lean red meat or iron-rich plant sources (beans, lentils, fortified cereals) and take a prenatal vitamin that contains vitamin A as beta-carotene if needed (not high-dose retinol) under your provider’s advice.
Practical tip: Avoid fish liver oil supplements (cod liver oil) unless your doctor approves.
Quick safety checklist (printable)
- ✅ Avoid alcohol entirely. ACOG
- ✅ Reheat deli meats until steaming or avoid them. CDC
- ✅ Skip raw fish, undercooked meats, raw eggs and raw sprouts. Mayo Clinic+1
- ✅ Eat 8–12 oz/week of low-mercury fish (salmon, sardines). U.S. Food and Drug Administration
- ✅ Limit caffeine to <200 mg/day. ACOG
Eating out, travel & cultural foods — practical tips
- Ask questions. Ask if cheeses are pasteurized, if fish is fully cooked, or if deli meats are heated. Servers expect these questions. nhs.uk+1
- Street food: In places where sanitation is uncertain, favor hot, freshly cooked meals and avoid pre-cut fruit from street stalls. U.S. Food and Drug Administration
- Air travel: Pack safe snacks (yogurt made from pasteurized milk, cooked chicken, bananas) for flights.
- If you get sick: Call your prenatal provider for fever, severe GI symptoms, or flu-like symptoms after eating a risky food (especially for concerns about Listeria). Early reporting is important. Mayo Clinic+1
What if I accidentally ate something I shouldn’t have?
Don’t panic — one exposure does not necessarily mean harm. Steps to take:
- Note what and when you ate it.
- Watch for symptoms (fever, muscle aches, diarrhea, severe abdominal pain). Call your prenatal provider if you get symptoms or if you’re worried — they may advise testing or monitoring. In some exposures (e.g., known listeria recall), your provider may recommend additional steps. CDC+1
Grocery list: safe swaps / shopping shorthand
- Replace deli cold cuts with: roasted chicken breast (hot), canned salmon (drained), or hummus + grilled veggies.
- Replace soft unpasteurized cheeses with: pasteurized mozzarella, cheddar, or cream cheese. nhs.uk
- Replace raw-egg recipes with: pasteurized egg products or store-bought dressings. Mayo Clinic
- Low-mercury fish options to buy: salmon, trout, sardines, pollock. U.S. Food and Drug Administration
Short FAQ (fast answers)
Q: Can I eat sushi?
A: Avoid raw-fish sushi/sashimi. Cooked sushi (e.g., shrimp tempura, eel that’s cooked) or vegetable rolls are safer. CDC
Q: Is soft-serve ice cream OK?
A: Only if made from pasteurized milk. If in doubt about pasteurization or machine cleanliness, skip. U.S. Food and Drug Administration
Q: How much caffeine is safe?
A: Generally limit to less than 200 mg/day during pregnancy (check coffee size and specialty drinks). ACOG
Q: Are pasteurized soft cheeses safe?
A: Yes — if the label specifically says “pasteurized,” they are considered safe. nhs.uk
Authoritativeness & sources (E-E-A-T)
This article summarizes guidance from leading authorities on pregnancy and food safety, including ACOG (American College of Obstetricians & Gynecologists), CDC, FDA, NHS, and major clinics (Mayo Clinic, Cleveland Clinic). Key source links used in this guide: ACOG on nutrition & alcohol, CDC on safer food choices and listeria, FDA fish/mercury guidance, NHS on foods to avoid, and Mayo Clinic on cooking/symptom advice. Mayo Clinic+5ACOG+5ACOG+5
Final notes
You’re feeding two (or more!) now — not everything on your plate needs to change, just a few sharp switches. Follow these swaps and safety tips, chat with your prenatal provider for anything specific, and enjoy eating well and safely. 💚
Sources (select official links used above)
(A few of the most important source pages I used — full list available on request.)
- CDC — Safer food choices for pregnant women. CDC
- FDA — Advice about eating fish (mercury guidance). U.S. Food and Drug Administration
- ACOG — Alcohol & pregnancy / Nutrition during pregnancy. ACOG+1
- NHS — Foods to avoid in pregnancy. nhs.uk
- Mayo Clinic — Pregnancy nutrition & food poisoning info. Mayo Clinic



Leave a Reply